Implantable Defibrillators ICD
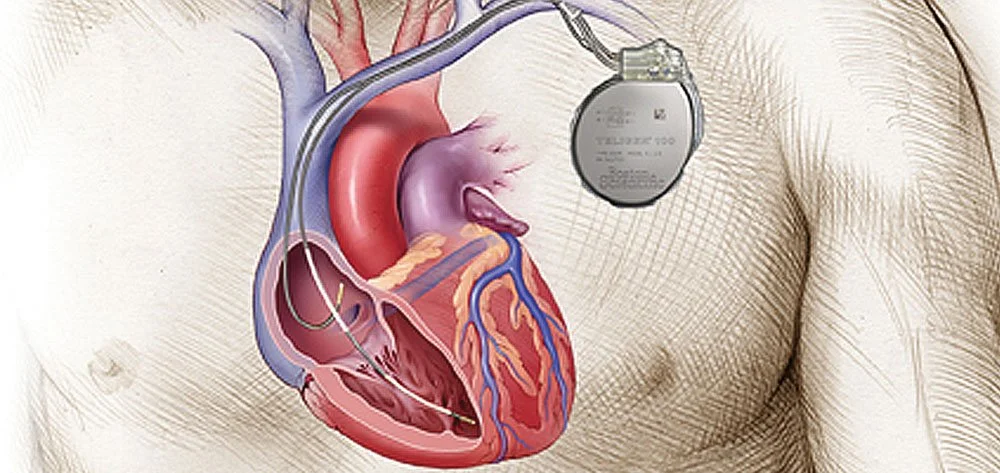
An implantable cardioverter-defibrillator (ICD) is a specialized device designed to directly treat many dysrhythmias, and it is specifically designed to address ventricular tachyarrhythmias. ICDs have revolutionized the treatment of patients at risk for sudden cardiac death due to ventricular tachyarrhythmias. A permanent pacemaker is an implanted device that provides electrical stimuli, thereby causing cardiac contraction when intrinsic myocardial electrical activity is inappropriately slow or absent. See the image below. All modern ICDs also function as pacemakers.
Why do I need a Defibrillator?
Indications for ICD implantation can be divided into two broad categories: secondary prophylaxis against sudden cardiac death and primary prophylaxis. For secondary prophylaxis, ICD placement is indicated as initial therapy in survivors of cardiac arrest due to ventricular fibrillation (VF) or hemodynamically unstable ventricular tachycardia (VT). Published guidelines exclude cases in which there are “transient or reversible causes,” [1] although in the specifics of its application this exclusion is somewhat controversial.
What are the complications of a Defibrillator?
Overall Defibrillators are relatively safe. Generally one can divide up the potential complications into three categories.
1. During the implant process, there is a risk when getting into the vein under the shoulder blade of puncturing the lung which lies very close to the vein, or an artery. This is not an uncommon occurrence but rarely leads to any ongoing problems, although very occasionally leads to partial collapse of the lung requiring aspiration of air form this area. This is a simple process. Whilst advancing and positioning the defibrillator leads, there is a very small risk (estimated at less than 1 in a 1000) of causing a small perforation in the heart. Similarly, this rarely causes any ongoing issues and is normally self limiting. Depending on the patient, there is a risk of bruising and bleeding, particularly if patients are on blood thinning medications, although again this is usually self limiting and can usually be dealt with at the time of the procedure.
2. Following successful defibrillator implantation, despite excellent lead positioning and contact with the heart, there remains an incidence of the leads moving such that either the next day or up to approximately one month, on testing they are no long in adequate contact with the heart. This is a nuisance and is easily dealt with by reopening the defibrillator implant and repositioning the defibrillator lead. The occurrence of this is very variable but is estimated to be between 5 and 10%.
3. The most feared complication of any defibrillator implant is infection and every precaution is made before, during and after the defibrillator implant of avoiding an infection. The incidence of this is extremely low but if the defibrillator or defibrillator leads do become infected then it is likely they will need to be removed.
How does a Defibrillator work?
All modern ICDs are equipped with a demand pacing system and serve the dual functions of emergency defibrillation and backup pacing. If a patient has a ventricular ICD and the device senses a ventricular rate that exceeds the programmed threshold, the device may be programmed to deliver antitachycardia pacing therapy (ATP) or defibrillation. With antitachycardia pacing, the device delivers a preset number of rapid pulses in succession in an attempt to terminate the ventricular tachycardia. If antitachycardia pacing therapy is ineffective within a prespecified number of trials or a prespecified time period, or if the ventricular rate exceeds a preset rate, the device delivers a high-energy electric shock to reset the heart’s electrical activity.
How is a Defibrillator implanted?
Defibrillators and Pacemakers are implanted either under local or general anaesthetic. Generally the procedure is fairly simple. Under sterile conditions, either on the right or the left, a small incision is made under the collar bone. Through this, the vein that leads directly to the heart is accessed and one or two defibrillator leads are put into this vein and advanced to particular parts of the heart, usually one in the atrium (top chamber) and one in the ventricle (bottom chamber). These leads will be carefully positioned and tested to ensure adequate positioning. The leads are then attached to the “generator” and this is positioned underneath the skin through the small incision previously made. The wound is closed, usually with dissolvable stitches, and a dressing is applied. This process may take half an hour to 2 hours depending on different circumstances.
What to expect after the Defibrillator is implanted?
You will remain in hospital overnight and be discharged the next morning. It is likely you will have some discomfort in the area the defibrillator is placed and also some bruising is likely. A dressing will be placed over the wound and you should try and keep the area dry for about a week. For the first two weeks after Defibrillator implantation you are not allowed to drive and should minimize use of the arm on the side that the Defibrillator was implanted. You should avoid using the arm above shoulder level and try and avoid sleeping on the left hand side. Arrangements will be made to check the wound and repeat the pacemaker tests after about 2 weeks.
What is involved with Defibrillator follow up?
Once a successful defibrillator implantation has been performed an initial wound check is usually made 2-4 weeks later and the defibrillator is interrogated to ensure it is functioning normally. Once this has occurred, after approximately one month it is very unusual for the leads to move. Subsequent follow up usually occurs approximately every six months and takes approximately 5-10 minutes. A pacemaker technician will interrogate the device for any abnormalities that it may have detected, for the defibrillator settings to make any changes and to assess correct function and the status of the batteries. Depending on the defibrillator device itself and the positioning of the leads, most defibrillator batteries will last 5-10 years. Through regular follow up it is possible to accurately predict the life left in the battery and when appropriate arrangements will be made to change the defibrillator generator, which is a fairly simple process.